CAUSES AND TREATMENET OF BACK PAIN

Back Pain is a common condition, and its symptoms can vary depending on the cause. The pain may be described as dull, sharp, throbbing, stabbing, aching, or searing. It can be constant or it may come and go or worsen with exercise or prolonged sitting.
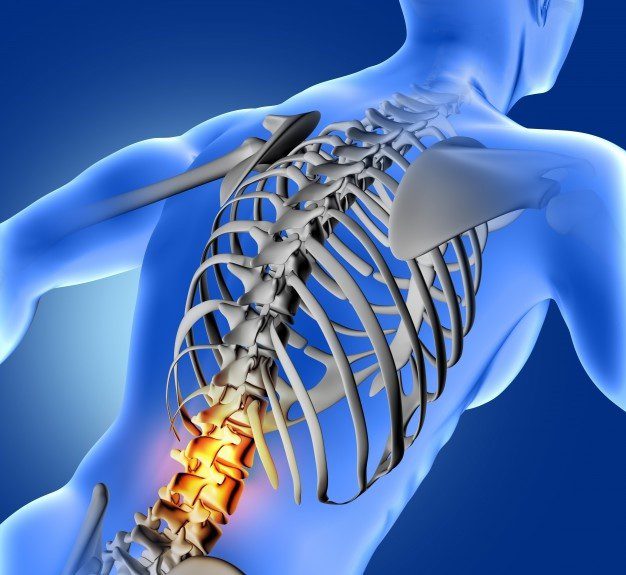
Lower back pain, sometimes called lumbago, is not a specific disease diagnosis. It’s a symptom of several different types of medical problems. It usually results from a problem with one or more parts of the lower back, such as:
- Ligaments and muscles
- Intervertebral discs
- Nerves
- The bony structures that make up the spine, called vertebral bodies or vertebrae
As frustrating as back pain can be, it will usually resolve or improve with rest within a few weeks. More severe conditions may require ongoing care and treatment, including surgery.
COMMON CAUSES:
There are many possible causes of back pain. Here are some of the more common:
- STRAIN OR SPRAIN
Strains and sprains are the most common causes of back pain, especially in the lower back. A strain refers to the tearing of a muscle or tendon (which connect muscles to bones), while a sprain refers to the tearing of a ligament (which connects bones in a joint).
A torn tendon or ligament may result from a fall or sports injury, or from overuse of a joint, know as a repetitive stress injury. The pain can range from mild to severe and is often described as an “all over pain” that moves into the buttocks. The pain tends to worsen with movement and improve with rest. Along with pain, muscle stiffness, muscle spasms, and a reduced range of motion are common.
- BULGING OR RUPTURED DISC:

Intervertebral discs are located between the bones of the spine and serve as shock-absorbing cushions. The discs can break down over time due to aging, trauma, obesity, repetitive stress, and smoking. When this happens, a disc can start to protrude outward, which is known as a bulging or slipped disc. The disc can also tear, resulting in a ruptured (herniated) disc. When this happens, the inner part of the disc (called the nucleus pulposus) will push out and compress neareby nerves, triggering nerve pain.
A ruptured disc in the low bck can cause sharp pain that may move down into the buttocks, groin, and leg. A ruptured disc in the neck can cause pain that moves down an arm. It may also cause muscle weakness, numbness, and tingling.
- OSTEOARTHRITIS:
Spine osteoarthritis is a form of arthritis that is caused by the wear and tear of cartilage between the spinal bones. As the cartilage wears away, you can experience a dull, aching, or throbbing pain that worsens with movement. You can feel a popping sensation known as crepitus, joint stiffness, and a reduced range of motion.
As the disease progresses, bony growths can develop. These bone spurs can compress nearby nerve roots, causing numbness and tingling sensations similar to that of a ruptured disc.
- SCIATICA:
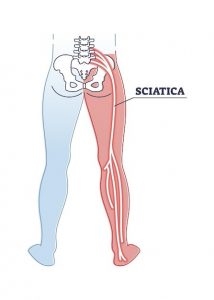
Sciatica refers to feeling on nerve pain that goes down the leg. The term is misnomer since the sciatic nerve (a large nerve in the leg that’s formed by nerve roots that come off of the lumbar spine) isn’t specifically irritated in this condition. Irritation of the lumbar nerve roots causes sciatica.
Sciatica causes shooting, burning, or cramping pain that extends from the lower back into a buttock and sometimes down the leg an into the sole of the foot. Tingling, numbness, and muscle weakness are common.
- SPINAL STENOSIS:
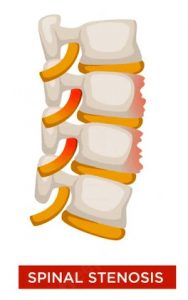
As you get older, the spinal canal, which contains the spinal cord, can begin to narrow. This is referred to as spinal stenosis. Spinal arthritis can also cause overgrowth of bone within the canal. If your spinal canal becomes too tight and compresses nerves, you can feel shooting pains in your lower back and buttock, muscle weakness, numbness, and tingling.
- SPONDYLOYSIS AND SPONDYLOLISTHESIS:

Spondylolysis is a stress fracture in one of the bones of the spine. It is most common in children who pay sports that put repeated stress on the lower back (such as gymnastics or football). Spondylolysis can also be due to a spinal injury or aging – related weakness of the spine. If the fracture weakens the spine too much, the vertebra may start to “slip,” leading to a condition called Spondylolysis. Symptoms of spondylolisthesis include pain and stiffness. If the slipped bone pinches a nerve, it can cause shooting pain, tingling, numbness, and weakness.
- OSTEOPOROSIS:
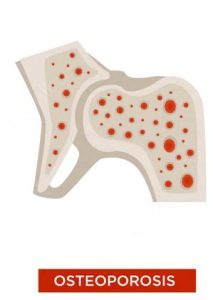
Osteoporosis is the thinning and weakening of the bones. Back pain associated with osteoporosis is most often due to compression fracture in the spinal column. The break can occur without warning, often after doing something as simple as sneezing or bending over.
- SCOLIOSIS:
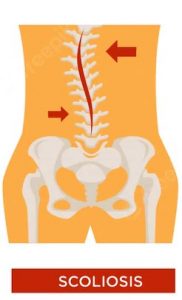
Scoliosis is a condition in which the spine curves or twists like the letter “S” or “C”. It usually develops in childhood. In most cases, the cause is unknown, although it is linked to conditions like cerebral palsy and muscular dystrophy. It can also result from a birth defect or family genetics (As multiple family members are sometimes affected). Scoliosis can cause chronic back or neck pain, as well as reduced range of motion. In severe cases, a person may begin to have trouble breathing.
RARE CAUSES
Less commonly, back pain is caused by systemic (Whole-body) disease, like:
- ANKYLOSING Spondylolysis:
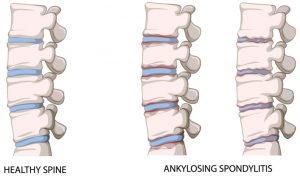
Ankylosing Spondylities is an inflammatory disease that causes the small bones of the spine to fuse together. This leads to lower back pain, spinal stiffness, and a hunched posture, often before the age of 40. The back pain tends to improve with exercise and worsen at night.
- CANCER:
A cancerous tumour in the spine may arise on its own or can be caused by the spread of cancer from other parts of the body (Called Metastasis). The pain is often described as gnawing and tends to worsen at night. The pain may radiate to the shoulders or neck and it can be accompanied by unexplained weight loss and chronic fatigue.
- OSTEOMYELITIS:

An infection in the spine, call osteomyelitis, causes severe, constant pain. It can occur due to recent spinal surgery or when a local infection (such as a staph infection) enters the bloodstream. Unlike most infection, fever is not common.
- CAUDA EQUINA SYNDROME:
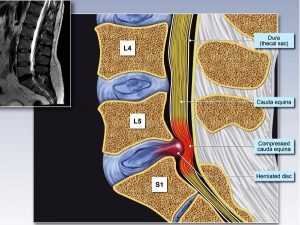 Cauda equine syndrome is a rare disorder that is caused by severe compression of spinal nerve roots in the lower spine. Besides lower back pain, it can cause numbness or tingling that spreads down one or both legs. Other symptoms include food drop (difficulty lifting the front of a foot) and problems with bladder or bowel control.
Cauda equine syndrome is a rare disorder that is caused by severe compression of spinal nerve roots in the lower spine. Besides lower back pain, it can cause numbness or tingling that spreads down one or both legs. Other symptoms include food drop (difficulty lifting the front of a foot) and problems with bladder or bowel control.
DIAGNOSIS:
The diagnosis of back pain starts with a review of your medical history and physical exam. You will be asked when the pain started, what it feels like, what makes the pain better or worse, and what other symptoms you have (such as numbness or swelling).
- PHYSICAL EXAM:
During your exam, your doctor will gently press on muscles and parts of the spine on or near the site of your pain. You will be asked to describe the location and type of pain. You will have a neurological exam to assess your nerve and motor responses. The aim of the exam is to identify any areas of sensory changes, muscle weakness, or reflex changes.
- LAB TESTS:
– A complete blood counts (CBC), including a white blood cell count (WBC) to detect signs of infection.
– Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) to detect signs of inflammation.
– HLA-B27 test to detect genetic signs of ankylosing spindylitis.
– Alkaline phosphatise (ALP) and lactate dehydrogenase (LDH) tests to help detect certain types of bone cancer.
- IMAGING TESTS:
Imaging tests are generally routinely needed nowadays. Magnetic resonance imaging (MRI) is usually the test of choice, with a computed tomography (CT) scan being the alternative. If the pain persists for several weeks or if muscle weakness is getting worse, imaging tests may be needed.
- DIFFERENTIAL DIAGNOSES:
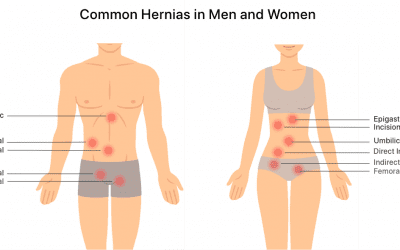
As part of your assessment, your doctor will consider other medical conditions that can cause back pain. The differential diagnosis will be based on your medical history and your risk factors for certain diseases. In the end, your back pain may be a part of a condition that doesn’t directly involve the back muscles or spine.
Example include:
- Abdominal aortic aneurysm
- Endometriosis
- Gallbladder disease
- Kidney infection
- Pancreatitis
- Pelvic inflammatory disease (PID)
- Peptic ulcer disease
- Prostatitis
- Shingles
TREATMENT:
The treatment of back pain often takes time. Most people recover by resting and avoiding activities that stress the lower back. Other treatments may be used to ease pain and restore the function of the spine or back muscles.
- SELF-CARE:
Rest, ice application and heat application can help ease back pain and possible speed the healing process. Ice can help reduce swelling while heat promotes blood flow and helps relax tissues.
- MEDICATIONS:
If rest and ice / heat application are not enough to ease your pain medications may be prescribed. Two of the most common are over-the – caounter nonsteroidal anti-inflammatories (NSAIDs) and prescription muscle relaxants. Epidural spinal injections, in which steroids are injected into the space around your spine, may be used to treat sciatica and spondylolisthesis. For spine osteoarthritis, a steroid injection into the spinal joint can be used if the pain is severe.
- PHYSICAL THERAPY:
Your doctor may also advise physical therapy to help strengthen and stretch your back muscles, improve mobility, and ease back pain. Low-impact exercise like walking, swimming, or biking can help improve your range of motion and flexibility.
- SPINAL SURGERY:
Spinal surgery is reserved for people who don’t get adequate symptom reliefe with non – operative treatment and the pain is well explained by the imaging studies. There are some conditions for which surgery may be beneficial, such as conditions that undermine the stability of the spine. A spine surgeon can help you determine if surgery is the right option for you and what risks are involved.
PREVENTION:
Back pain is one of the most common ailments affecting people of all ages. There are ways to prevent it of keep it from worsening.
Some of the more useful prevention tips include:
- Maintaining a healthy weight
- Exercising regularly with low-impact activities to strengthen core muscles.
- Practicing good posture and body mechanics.
- Sleeping on a bed that supports the spine
- Quitting cigarettes (chemicals in tobacco smoke promote the deterioration of spinal disks)
WHEN TO SEE A DOCTOR:
Most cases of back pain last for a few days and resolve completely within a few weeks. If you have sudden, new back pain, you should contact you doctor.
There are a few warning signs that immediate care is needed:
- The pain persists for more than a few days or is worsening.
- The pain wakes you up at night.
- You have a fever, chills, or other signs of infection.
- You have problems with bladder or bowel control.
DEPARTMENT OF ORTHOPEDICS, TRAUMA, SPINE & JOINT REPLACEMENT SURGERY
Departments
- Department Of Cardiology
- Neurology
- Nephrology
- Urology
- Spine Surgery
- Orthopaedics/ Trauma
- General Medicine
- General and Laparoscopic Surgery
- Gastrointestinal Surgery
- Bariatric And Diabetes Surgery
- Intensive Care/ Critical Care
- Pulmonology
- Obstetrics and Gynecology
- Oral and maxillofacial surgery
- Dental and Implant surgery
- Neuro Surgery
- Radiology
- Physiotherapy