Parkinson’s disease | Modified
Parkinson’s disease is a progressive neurodegenerative disorder prevalent worldwide and affecting all ethnic groups.
It is a common cause of morbidity amongst the elderly and leads to overall poor quality of life. With improvement in medical care and longer life expectancy, the prevalence of this ailment is rising.
The age of onset ranges from 45 to 80 years but most of the patients present in 6th or 7th decade. In the majority of the patients, the cause of the disease remains unknown.
In Parkinson’s disease, a certain group of brain cells gradually break down or die. Clinical symptoms are due to a loss of neurons that produce a chemical messenger called dopamine. When dopamine levels decrease, it causes abnormal brain activity, leading to impaired movement and other symptoms of Parkinson’s disease.
The cause of Parkinson’s disease is unknown, but several factors appear to play a role, including:
- Genes: Research has shown certain specific genetic mutations to be associated with Parkinson’s disease. But these occur in rare cases with many family members affected by Parkinson’s disease.
- Certain gene variations appear to increase the risk of Parkinson’s disease.
- Environmental triggers: Exposure to certain toxins or environmental factors may increase the risk of later Parkinson’s disease, but the risk is relatively small.
Abnormal protein deposition in brain cells
- Lewy bodies: Clumps of specific substances within brain cells are microscopic markers of Parkinson’s disease. These are called Lewy bodies, and researchers believe these Lewy bodies hold an important clue to the cause of Parkinson’s disease.
- Alpha-synuclein is found within Lewy bodies: Although many substances are found within Lewy bodies, scientists believe an important one is a natural and widespread protein called alpha-synuclein (a-synuclein). It’s found in all Lewy bodies in a clumped form that cells can’t break down. This is currently an important focus among Parkinson’s disease researchers.
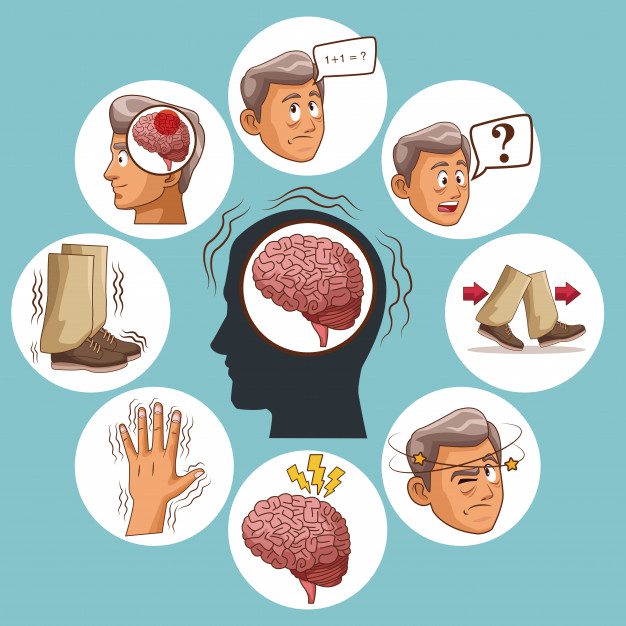
Symptoms
- Rest tremor: One of the most prominent and early symptoms. Tremors are usually the reason behind the patient seeking consultation. Thumb and wrist movement lead to classical ‘ Pin rolling ‘. They are usually brought to notice by a relative. One side of the body is usually more affected than the other. Tremors predominantly appear at rest and get relieved during activity and sleep. Rarely patient has difficulty inactivity due to tremor.
- Bradykinesia: Bradykinesia remains the pathognomonic feature of Parkinson’s disease. Patients notice that they require more time to perform activities of daily living. They complain of difficulty initiating movement. In advanced stages, there is akinesia i.e inability of the body to initiate volitional movement.
- Rigidity: There is a cogwheel type of rigidity affecting extremities. This can be elicited with passive movement of limb muscles and activated by asking the patient to move the contralateral limb. The patient complains of difficulty in changing posture while sleeping.
- Impaired posture: There is progressive stooping of posture. Advanced disease is associated with recurrent falls. There is a reduced arm swing with short steps. Classical ‘Festinant’ gait consists of a gradual increase in speed while patients try to catch their center of gravity.
- Mask facies: Staring look with reduced eye blinking and lack of expression over the face.
- Low volume and monotonous speech.
- Change of handwriting with progressive diminution of alphabet size and changes in signature
Complications:
- Parkinson’s disease is often accompanied by these additional problems, which may be treatable:
- Dementia and cognitive impairment: These usually occur in the later stages of Parkinson’s disease and respond poorly to medications.
- Swallowing difficulty: usually seen in advanced stages of the disease. Saliva may pool in your mouth due to slowed swallowing, leading to drooling. This pooling of saliva may lead to aspiration pneumonitis and is a common cause of morbidity in later stages of the disease.
- Chewing and eating problems: Late-stage Parkinson’s disease affects the muscles in your mouth, making chewing difficult. This can lead to choking and poor nutrition.
- Sleep problems and sleep disorders: People with Parkinson’s disease often have sleep problems, including waking up frequently throughout the night, waking up early, or falling asleep during the day.
- People may also experience rapid eye movement sleep behavior disorder, which involves acting out your dreams. Medications may help your sleep problems.
- Bladder problems: Parkinson’s disease may cause bladder problems, including being unable to control urine or having difficulty urinating.
- Many people with Parkinson’s disease develop constipation, mainly due to a slower digestive tract.
DIFFERENT STAGES OF PARKINSON’S DISEASE:
Each person with Parkinson’s disease experiences symptoms in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early-stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:

- EARLY-STAGE:
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notice some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement (nor arm swing when walking) slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
- MID-STAGE:
Symptoms start getting worse. Tremor, muscle stiffness, and movement problems may now affect both sides of the body. Balance problems and falls are becoming more common. You may still be fully independent but daily tasks of everyday living, such as bathing and dressing, are becoming more difficult to do and take longer to complete.
- MID-LATE STAGE:
Standing and walking are becoming more difficult and may require assistance with a walker. You need full-time help to continue to live at home.
ADVANCED STAGE:
You now require a wheelchair to get around or are bedridden. You may experience hallucinations or delusions. You now require full-time nursing care.
DIAGNOSIS
No specific test exists to diagnose Parkinson’s disease. The neurologist will diagnose Parkinson’s disease based on clinical history, review of signs and symptoms, and a neurological and physical examination.
A blood test and MRI scan may be ordered by a treating Neurologist to rule out conditions that mimic Parkinson’s Disease.
SPECT and DaT scans are now available to provide support to clinical diagnosis.
Trial of Levodopa / Carvidopa ( anti- Parkinson medication ) may be used by treating neurologist. Significant improvement with this medication will often confirm your diagnosis of Parkinson’s disease.
Sometimes it takes time to diagnose Parkinson’s disease. Doctors may recommend regular follow-up appointments with neurologists trained in movement disorders to evaluate your condition and symptoms over time and diagnose Parkinson’s disease.
Diagnosis
No specific test exists to diagnose Parkinson’s disease. The neurologist will diagnose Parkinson’s disease based on clinical history, review of signs and symptoms, and a neurological and physical examination.
A blood test and MRI scan may be ordered by the treating Neurologist to rule out conditions that mimic Parkinson’s Disease.
SPECT and DaT scans are now available to provide support to clinical diagnosis.
A trial of Levodopa / Carbidopa ( anti- Parkinson medication ) may be used by treating neurologists. Significant improvement with this medication will often confirm your diagnosis of Parkinson’s disease.
Sometimes it takes time to diagnose Parkinson’s disease. Doctors may recommend regular follow-up appointments with neurologists trained in movement disorders to evaluate your condition and symptoms over time and diagnose Parkinson’s disease.
Treatment
Parkinson’s disease can’t be cured, but symptom relief can be achieved through medication leading to improved quality of life. In few selective patients with advanced disease, surgery may be advised.
Non-Pharmacological Approach
DIET: Diet high in fiber with adequate liquids prevents constipation. Food rich in Omega 3 fatty acids is beneficial.
EXERCISE: Exercising may increase your muscle strength, flexibility, and balance. Exercise can also improve your well-being and reduce depression or anxiety.
Pharmacological Approach
Medications
- Carbidopa-levodopa.
Levodopa, the most effective Parkinson’s disease medication, is a natural chemical that passes into your brain and is converted to dopamine.
Levodopa is combined with carbidopa (Lodosyn), which protects levodopa from early conversion to dopamine outside your brain. This prevents or lessens side effects such as nausea.
Side effects may include nausea or lightheadedness (orthostatic hypotension).
- Carbidopa-levodopa infusion.
Duopa is a brand-name medication made up of carbidopa and levodopa. However, it’s administered through a feeding tube that delivers the medication in a gel form directly to the small intestine.
Duopa is for patients with more advanced Parkinson’s who still respond to carbidopa-levodopa, but who have a lot of fluctuations in their response. Because Duopa is continually infused, the blood levels of the two drugs remain constant.
Placement of the tube requires a small surgical procedure. Risks associated with having the tube include the tube falling out or infections at the infusion site.
- Dopamine agonists.
Unlike levodopa, dopamine agonists don’t change into dopamine. Instead, they mimic dopamine effects in your brain. They last longer and may be used with levodopa to smooth the sometimes off-and-on effect of levodopa.
Dopamine agonists include pramipexole, ropinirole, and rotigotine. Apomorphine is a short-acting injectable dopamine agonist used for quick relief.
- MAO B inhibitors.
These medications include selegiline, rasagiline, and safinamide. They help prevent the breakdown of brain dopamine by inhibiting the brain enzyme monoamine oxidase B (MAO B). This enzyme metabolizes brain dopamine. Selegiline given with levodopa may help prevent wearing-off.
- Catechol O-methyltransferase (COMT) inhibitors.
Entacapone and opicapone are the primary medications from this class. This medication mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine.
- Anticholinergics.
These medications were used for many years to help control the tremor and Dystonia associated with Parkinson’s disease.
- Amantadine.
It provides short-term relief of symptoms of mild, early-stage Parkinson’s disease. It may also be given with carbidopa-levodopa therapy during the later stages of Parkinson’s disease to control involuntary movements (dyskinesia) induced by carbidopa-levodopa.
Surgical Procedures:
Deep brain stimulation
In deep brain stimulation (DBS), surgeons implant electrodes into a specific part of your brain. The electrodes are connected to a generator implanted in your chest near your collarbone that sends electrical pulses to your brain and may reduce your Parkinson’s disease symptoms.
Electrical pulse settings are adjusted as necessary. Surgery involves risks, including infections, strokes, or brain hemorrhage. Some people experience problems with the DBS system or have complications due to stimulation.
Deep brain stimulation is most often offered to people with advanced Parkinson’s disease who have unstable medication (levodopa) responses. DBS can stabilize medication fluctuations, reduce or halt involuntary movements (dyskinesia), reduce tremors, reduce rigidity, and improve slowing of movement.
DBS is effective in controlling erratic and fluctuating responses to levodopa or for controlling dyskinesia that doesn’t improve with medication adjustments.
However, DBS isn’t helpful for problems that don’t respond to levodopa therapy apart from a tremor. A tremor may be controlled by DBS even if the tremor isn’t very responsive to levodopa.
Although DBS may provide sustained benefits for Parkinson’s symptoms, it doesn’t keep Parkinson’s disease from progressing.
Because there have been infrequent reports that the DBS therapy affects the movements needed for swimming, the Food and Drug Administration recommends consulting with your doctor and taking water safety precautions before swimming.
Dr. Chetan Maniya
M.B.B.S., M.D.(General Medicine),
D.N.B. (Neurology)
Departments
- Department Of Cardiology
- Neurology
- Nephrology
- Urology
- Spine Surgery
- Orthopaedics/ Trauma
- General Medicine
- General and Laparoscopic Surgery
- Gastrointestinal Surgery
- Bariatric And Diabetes Surgery
- Intensive Care/ Critical Care
- Pulmonology
- Obstetrics and Gynecology
- Oral and maxillofacial surgery
- Dental and Implant surgery
- Neuro Surgery
- Radiology
- Physiotherapy